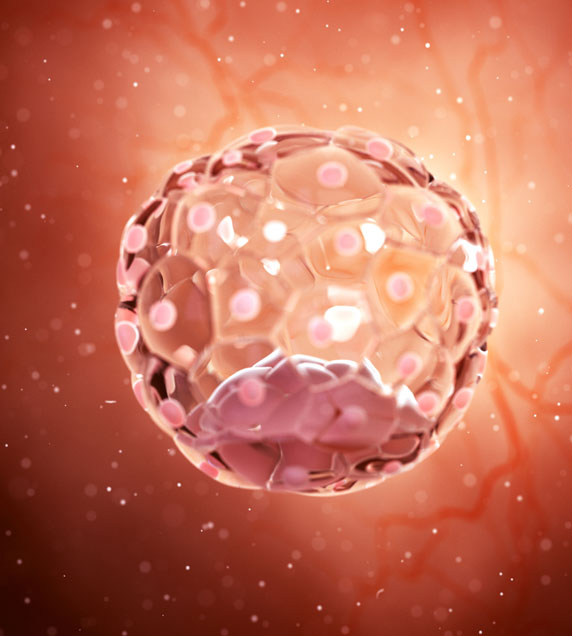
IVF or
In Vitro Fertilization
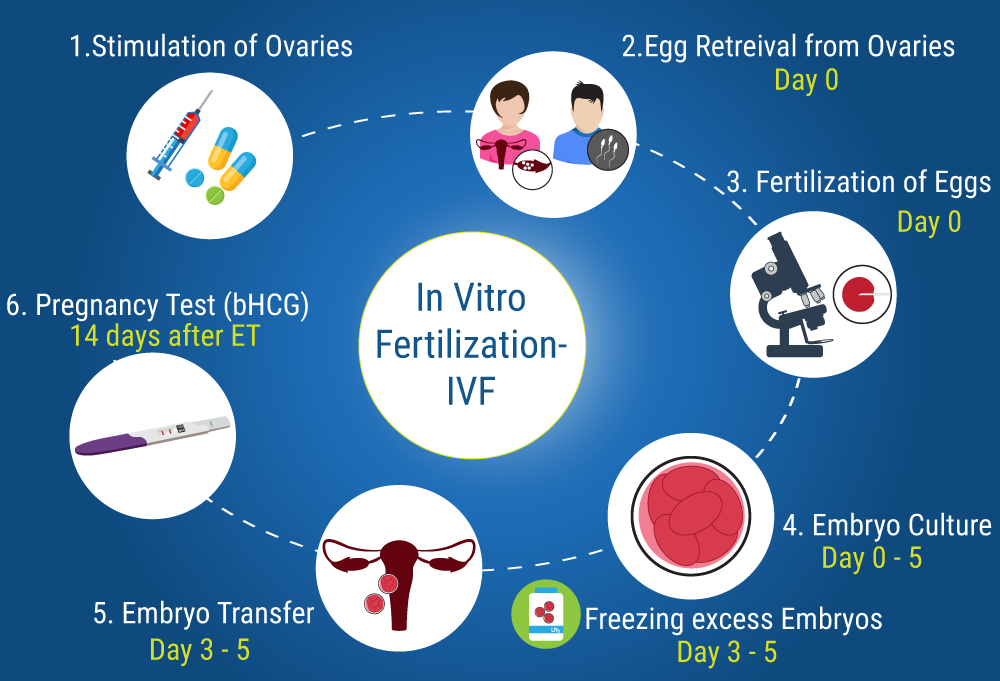
It is a process where fertilization occurs when an egg is fused with sperm, in vitro. Conception, in this case, takes place outside the human body, but once fertilization has taken place, the fertilized embryo is put back into the uterus.
IVF is an Assisted Reproductive Technique that helps couples conceive when non-invasive or minimally invasive procedures such as fertility drugs and IUI do not work.
It is one of the most common procedures used to treat various fertility issues like blocked fallopian tubes, ovulation disorders, endometriosis, ovarian failure, impaired sperm production etc.
What You can
Expect
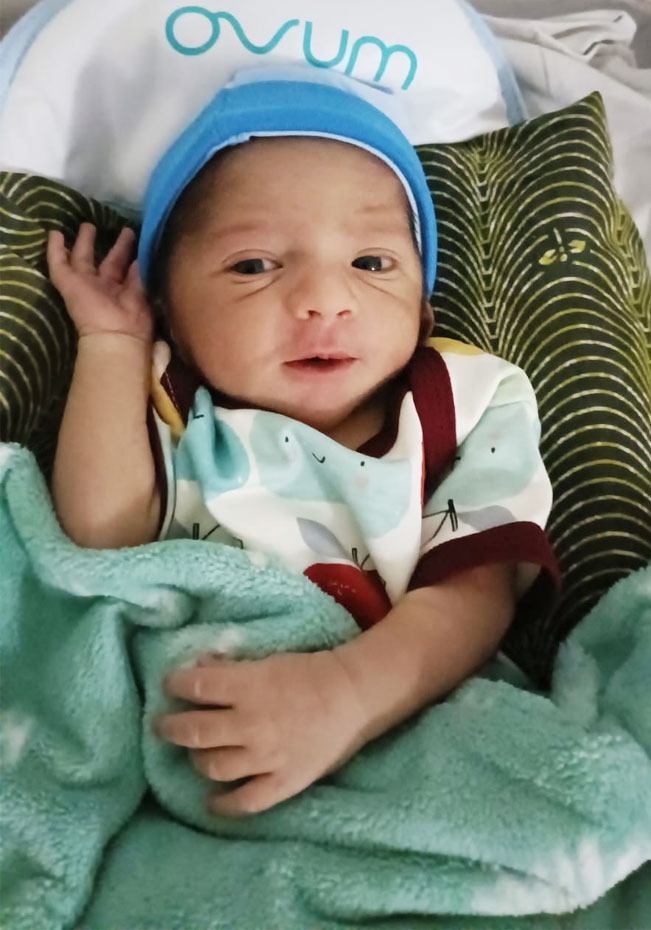
The IVF procedure begins 4 to 6 weeks prior to egg retrieval. Once fertilization takes place, the embryos are transferred approximately 3 to 5 days later.
A step by step process of the entire cycle is explained:
Result
In case of a positive outcome, the expectant mother is referred to an obstetrician for prenatal care approximately six to eight weeks after embryo transfer.
If the outcome is not positive, one can consult the doctor and go for a repeat IVF cycle or choose another method that may improve their chances of pregnancy.
Step One
Starting from Day 2 of the menstrual cycle the patient will need to undergo daily injections and ultrasound scans at regular intervals to monitor follicle growth. Ovarian stimulation may also be achieved with a combination of tablets and injections. In addition, blood tests are also done to monitor hormone levels. The uterine lining will be assessed at the time of the ultrasound scan.
Step Two
When the follicles reach the right size (18-20mm) as seen on the ultrasound scan by the IVF specialist, an injection called the trigger is given to mature the eggs
Step Three
The egg retrieval is scheduled 34 to 36 hours after administration of the trigger injection.
Step Four
On the day of oocyte retrieval the husband or partner will need to give a semen sample. There should be a period of abstinence of 2- 3 days before giving the sample. If the partner cannot be present or in case of difficulties in producing a sample on the day of egg retrieval, a semen sample is collected in advance and the semen analyzed and frozen for use during the IVF.
Step Five
The semen sample is processed and placed in a petri dish along with the retrieved eggs.
Step Six
Fertilization takes place and embryo development starts.
Step Seven
Embryos can be cultured in the lab for up to five days depending on their quality.
Step Eight
The embryo transfer may be done on any day between the second and fifth day after oocyte retrieval. By the fifth day the embryo is a blastocyst and having a blastocyst transfer can improve your chances of pregnancy. Generally, not more than two embryos are transferred but you can also opt for an elective single embryo transfer.
Step Nine
Two weeks after the date of embryo transfer a blood test is done to check for pregnancy
PRECAUTIONS TO BE
FOLLOWED
STAY HYDRATED
Drinking plenty of water also plays an important role in the success of IVF after embryo transfer.
EAT HEALTHILY
A healthy and balanced diet full of vitamins, minerals, iron, and zinc. Or you must go with green leafy vegetables and fresh fruits.
PROPER BED REST
You have to get proper sleep and rest after the embryo transfer because it will improve the chances of success of IVF. You must take some days off from your hectic working schedule so that you can take proper rest at home.

Combining IVF and
Donor Eggs
This process is a little bit different. You will first select an egg donor who is a healthy, young woman. She will undergo ovarian stimulation and egg retrieval because she will be providing the eggs for the IVF cycle. Alternatively, you may choose to use eggs that have already been retrieved and frozen at an egg bank.
Our embryologists will fertilize these eggs in the lab and you will undergo the embryo transfer.
We recommend IVF with donor eggs to women who have low egg quality or quantity. This can be due to age, certain medical treatments and fertility issues.
If you have questions about whether you should pursue IVF with your own eggs or donor eggs, contact us to schedule an appointment. We are happy to guide you through this important decision.
Recurrent IVF Failure
IVF can be very successful treatment methods. However, some cycles don’t finish with successful implantation, even after a number of transfers with apparently good embryos. Also, sometimes a cycle achieves a conception, but the pregnancy doesn’t develop to term.
There are various biological reasons why these two circumstances could be related, which lead us to look at potential therapies which
- Clotting (thrombophilia) screen – Small clots in the blood have been identified as a possible cause for a pregnancies failing to progress. In some cases this can be treated with aspirin, or heparin injections to thin the blood.
- Immune screen – Increased levels of uterine natural killer cells (white cells) and autoantibodies (antibodies attacking specific organs) have also been suggested as a cause for repeated failure of cycles. The use of steroids, intralipids and other drugs to suppress the immune system and to help a pregnancy develop are controversial. More clinical trials are needed to understand the ways in which the immune system affects pregnancy and which treatments might benefit which women). Some of the drugs used in these treatments have side effects for both a mother and her developing baby, and it’s important to understand these risks before deciding with your doctor whether testing or treatment is recommended.
Endometrial tests
- Hysteroscopy or endometrial scratch – We may suggest a hysteroscopy (passing a flexible telescope into the womb under general anaesthetic) if we suspect scar tissue formation or the presence of a fibroid or polyp inside the womb which needs to be removed. There is some evidence that this procedure itself, or performing an endometrial scratch, can increase implantation rates.
- Endometrial Receptivity Array – A small amount of tissue from the womb lining (endometrium) can be sampled and analysed for the presence of over 200 genes known to be associated with implantation. Studies have shown that for some women this “window of implantation” is shifted either earlier or later in the menstrual cycle, or it is very narrow. Furthermore, by moving the planned embryo transfer to the appropriate time, chances of successful implantation can be improved.
could help.
Paternal factors
- Sperm DNA fragmentation – Assessing the degree of damage to sperm DNA help identify those couples that would benefit from ICSI treatment.
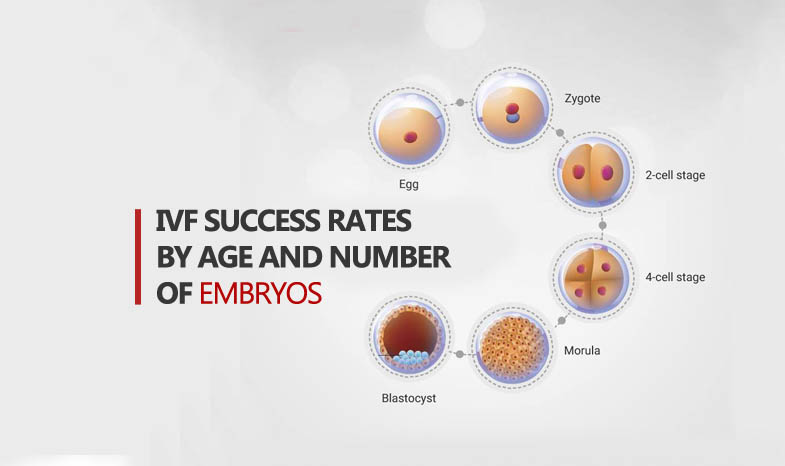
Embryo factors
- Genetic screening – We can use genetic screening to learn more about embryos before they are implanted, which helps us select the best embryos most likely to implant.
- Embryoscope™ (Time-lapse imaging) – Recording information by time-lapse photography allows us to assess more subtle changes seen during embryo development and identify the best embryos for transfer.
- Laser-assisted hatching – Assisted hatching is a physical or chemical treatment carried out immediately before embryo transfer. It weakens an area of the zona pellucida (the embryo’s ‘shell’) with the aim of improving the chances of implantation. We use a laser, as it is considered to be the safest and most accurate method.